Feeling Off Before Your Period? Let’s Talk About Why.
Have you ever felt off—more anxious, more emotional, or just not quite like yourself—only to realize a few days later that it was related to your menstrual cycle? You’re not alone. Many people notice that everyday stress feels heavier, emotions feel more intense, and even small things can feel overwhelming in the days leading up to their period.
In fact, around 80–95% of people who menstruate experience some premenstrual symptoms like bloating, fatigue, or cramps. But for about 20–40%, these monthly changes also come with noticeable emotional or mental health shifts. That’s where terms like PMS, PMDD, and PME come into play.
What Is PMS, PMDD, and PME?
Premenstrual Syndrome (PMS) includes one or more physical or emotional symptoms that occur during the two weeks leading up to your period—things like irritability, mood changes, breast tenderness, or fatigue. These symptoms can be uncomfortable but typically don’t interfere significantly with everyday functioning.
However, for some people, the emotional changes are more intense and can impact daily life. This may be a sign of Premenstrual Dysphoric Disorder (PMDD), a more severe form of PMS that involves mood shifts, anxiety, and depressive symptoms that occur cyclically and can be significantly distressing and impairing.
Then there’s Premenstrual Exacerbation (PME)—when an existing mental health condition such as depression, anxiety, OCD, or bipolar disorder worsens during the premenstrual phase. Unlike PMDD, PME doesn't involve new symptoms but rather intensifies what’s already present.
Understanding the Biological Connection
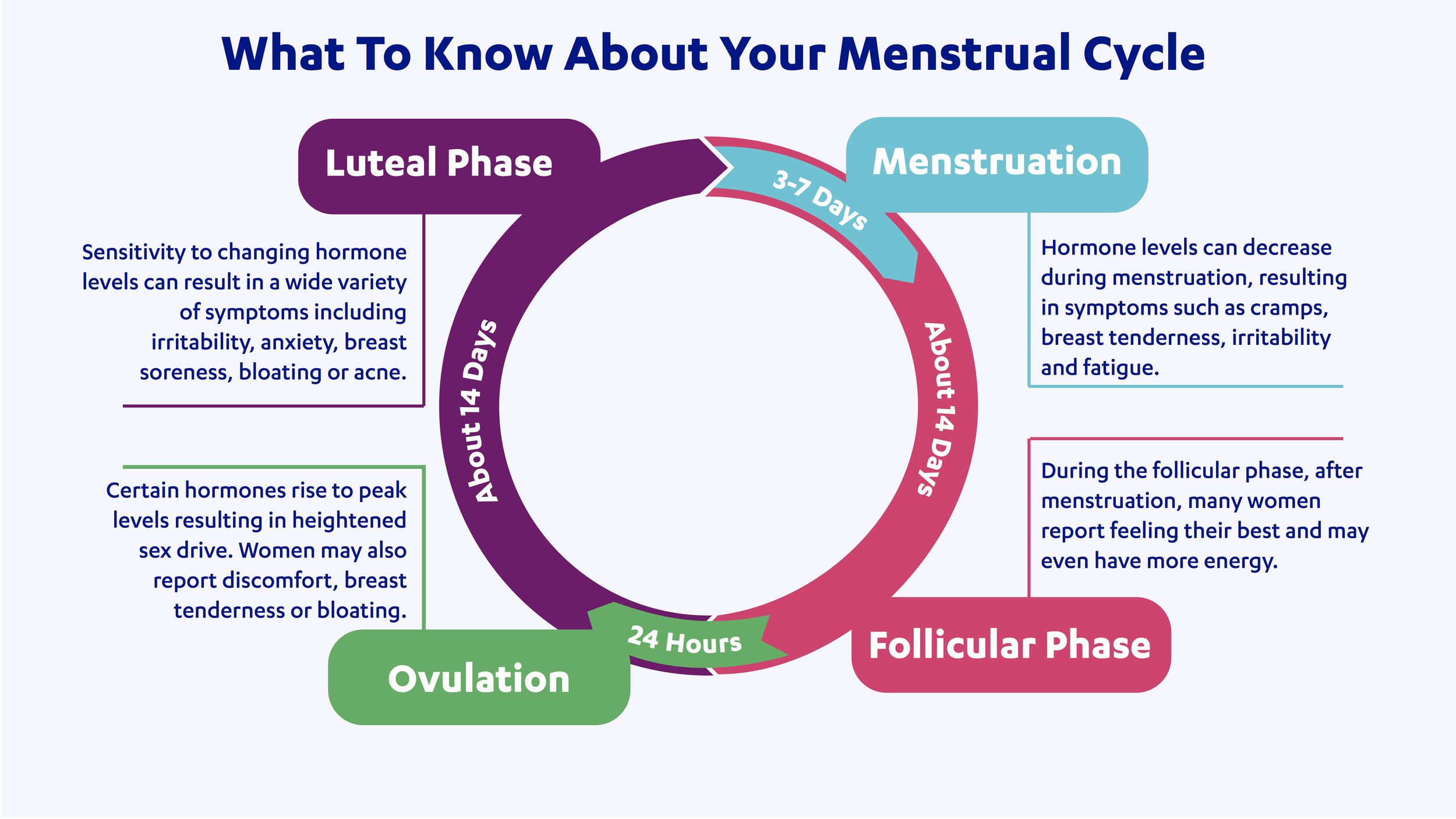
Hormonal shifts throughout the menstrual cycle—particularly in estrogen and progesterone—can influence brain chemicals like serotonin, dopamine, and GABA. These neurotransmitters play essential roles in mood regulation, motivation, stress response, and emotional balance.
When these hormone levels rise or fall, they can lead to emotional and physical changes. For those who are especially sensitive to these shifts, it can affect daily functioning in real, measurable ways.
This isn’t simply a matter of “feeling emotional”—it’s a complex biological response to internal chemical changes. For example, PMDD has been shown to involve differences in brain structure and function, especially in areas like the amygdala (involved in emotional regulation) and the prefrontal cortex (responsible for higher-order thinking and decision-making).
Menstrual Cycle Changes
What Causes PMDD?
The causes of PMDD are complex and multifactorial. While there's still more to learn, research suggests several key contributors:
Genetic Sensitivity – Some people have a genetic predisposition to be more sensitive to hormonal fluctuations, including variations in the estrogen receptor alpha gene.
GABA and Allopregnanolone – In the luteal phase (the second half of the cycle), progesterone rises, and so does Allopregnanolone, its calming metabolite that interacts with GABA receptors (which help regulate mood). People with PMDD may be more sensitive to changes in allopregnanolone, which can affect how the brain responds to stress and mood regulation during the menstrual cycle.
Low Estrogen and Serotonin – Estrogen helps maintain serotonin, the neurotransmitter involved in mood. When estrogen dips before menstruation, serotonin levels may also fall, particularly in those more sensitive to the shift.
Brain Structure and Stress Response – Research shows people with PMDD may have changes in areas like the amygdala, which regulates emotional response, and may also have a heightened stress response overall.
Hypothalamic-Pituitary-Adrenal (HPA) Axis – This system regulates how we respond to stress. A history of trauma, chronic stress, or adverse childhood experiences can influence HPA function and increase vulnerability to PMDD symptoms.
Treatment Approaches
The right treatment often depends on individual symptoms, medical history, and any co-occurring mental health conditions. A thorough evaluation with a healthcare provider—especially one who understands both hormonal health and mental health—can make a world of difference.
Here are a few options that may be helpful:
Non pharmacologic approaches include nutritional changes (reducing intake of caffeine, sugar, sodium, alcohol, and nicotine may ease symptoms), exercise, Cognitive Behavioral Therapy (CBT), and Acupuncture.
Medication options: SSRIs (Selective Serotonin Reuptake Inhibitors), hormonal contraceptives, and other hormonal treatments (in some severe cases, medications like GnRH analogues or even surgical options may be discussed—but these are typically reserved for complex or treatment-resistant cases and must be approached with care).
Support Starts With Awareness
If you’ve noticed that your mental health changes with your cycle, you’re not imagining things—and you’re not alone. These symptoms are common, biologically based, and worthy of understanding and care.
By learning more about how our hormones interact with our mood, behaviors, and physical symptoms and by continuing to push back against the stigma around menstrual mental health, we open the door to greater compassion, better treatment, and the possibility of feeling more in control of our wellbeing—every day of the month.